WHY AN UNCIRCUMCISED MALE STANDS THE RISK OF CONTRACTING HIV
WHY AN UNCIRCUMCISED MALE STANDS THE RISK OF CONTRACTING HIV
Many times I hear people ask and say so what if a man is not circumcised? That it has nothing to do with his ability to perform optimally when it comes to satisfying his partner. I did a personal research asking a group of circumcised male and uncircumcised male of their experience during sexual intercourse and found out that the disparity between them was not significant.
Over time many bodies ranging from WHO, UNAIDS and so on have continuously advised that it is of great importance to have male children circumcised as its reduces the risk of contracting HIV by half especially in Sub-Saharan Africa where some socio-cultural and religious belief hinders individuals from doing so.
Male circumcision reduces the risk that a man will acquire HIV from an infected female partner, and also lowers the risk of other STI’s, penile cancer, and infant urinary tract infection.
For female partners, male circumcision reduces the risk of cervical cancer, genital ulceration, bacterial vaginosis, trichomoniasis, and Human Papiloma Virus (HPV). Although male circumcision has risks including pain, bleeding, and infection, more serious complications are rare.
Biologic Plausibility
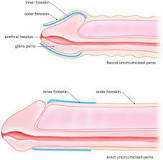
Compared with the dry external skin surface of the glans penis and penile shaft, the inner mucosa of the foreskin has less keratinization (deposition of fibrous protein) and a higher density of target cells for HIV infection. Some laboratory studies have shown the foreskin is more susceptible to HIV infection than other penile tissue, although others have failed to show any difference in the ability of HIV to penetrate inner compared with outer foreskin surface.
A ‘study’ published in the September issue of the American Journal of Pathology by researchers at Rush-Presbyterian-St. Luke’s Medical Center, Children’s Memorial Hospital and the University of Illinois at Chicago School of Public Health points to the biological mechanisms underlying this protective effect.
The researchers examined foreskin tissue obtained from eight children and six adults who were undergoing circumcision for other reasons. Those tissues were compared with cervical tissue, which served as controls. The analysis showed that foreskin mucosa (cells underneath the surface) contains high concentrations of the cells targeted by HIV. The foreskin tissue contained higher densities of CD4+ T cells, macrophages and Langerhans’ Cells (LC) in adults than in children or in cervical tissue. The highest proportion of these HIV target cells were found in men with a history of infection, which is consistent with studies finding that men with sexually transmitted infections are more susceptible to HIV.
According to Alan Landay, PhD, department of Immunology/Microbiology and at Rush-Presbyterian-St. Luke’s Medical Center, the higher the concentration of HIV target cells, the more susceptible the tissue is to HIV. This proved to be the case. When the authors introduced HIV to the tissue in culture, the cells in the foreskin tissues were infiltrated with HIV rapidly and at much greater intensity than the cervical tissue.
According to the first author, Bruce Patterson, M.D, viral pathologist in the division of Infectious Diseases at Children’s Memorial Hospital; there are logical, but as yet unproven theories explaining how HIV infection occurs in the circumcised penis. “Infection may occur through the urethral mucosa or through disruptions of the penile shaft epithelia caused by genital ulcer disease or trauma.
In some other research, evidence was needed to establish a causal relationship between lack of circumcision and HIV, so three randomized controlled trials were commissioned as a means to reduce the effect of any confounding factors. Trials took place in South Africa, Kenya and Uganda. All three trials were stopped early by their monitoring boards on ethical grounds, because those in the circumcised group had a lower rate of HIV contraction than the control group.
The results showed that circumcision reduced vaginal-to-penile transmission of HIV by 60%, 53%, and 51%, respectively. A meta-analysis of the African randomized controlled trials found that the risk in circumcised males was 0.44 times that in uncircumcised males. The authors also stated that using circumcision as a means to reduce HIV infection would, on a national level, require consistently safe sexual practices to maintain the protective benefits
I am of the opinion that regardless of the fact that a circumcised male has a low risk effect in contracting HIV when compared to an uncircumcised male; it should not be the only intervention. Other interventions should be continued and efficiently delivered to key populations as it is the total package which includes awareness on safe sex (condom use correctly and consistently), being faithful to one sexual partner, early detection and treatment of new HIV infections, prevention of mother to child transmission, prevention for intravenous drug users and most importantly abstinence which is still the best form of prevention today that would take us closer to our goal of an HIV free generation.